Time-in-Range: What’s an Achievable Goal with Diabetes?
By Adam Brown
.jpg) By Adam Brown
By Adam Brown
My approach to time-in-range goals, five key tips to spend more time-in-range each day, and what’s still to come from experts…
Q: “What do you think is an attainable percent time in range? My son’s doctor is happy about his A1c around 7.1%, and I think that can lead to being complacent or thinking he is good enough. What is a good goal for percent time in range on a daily basis?” – Madeline G.
Madeline – thank you for this important question! We love that you are thinking Beyond A1c. This is a big topic, so it is tackled in parts below.
How do we define “time-in-range”?
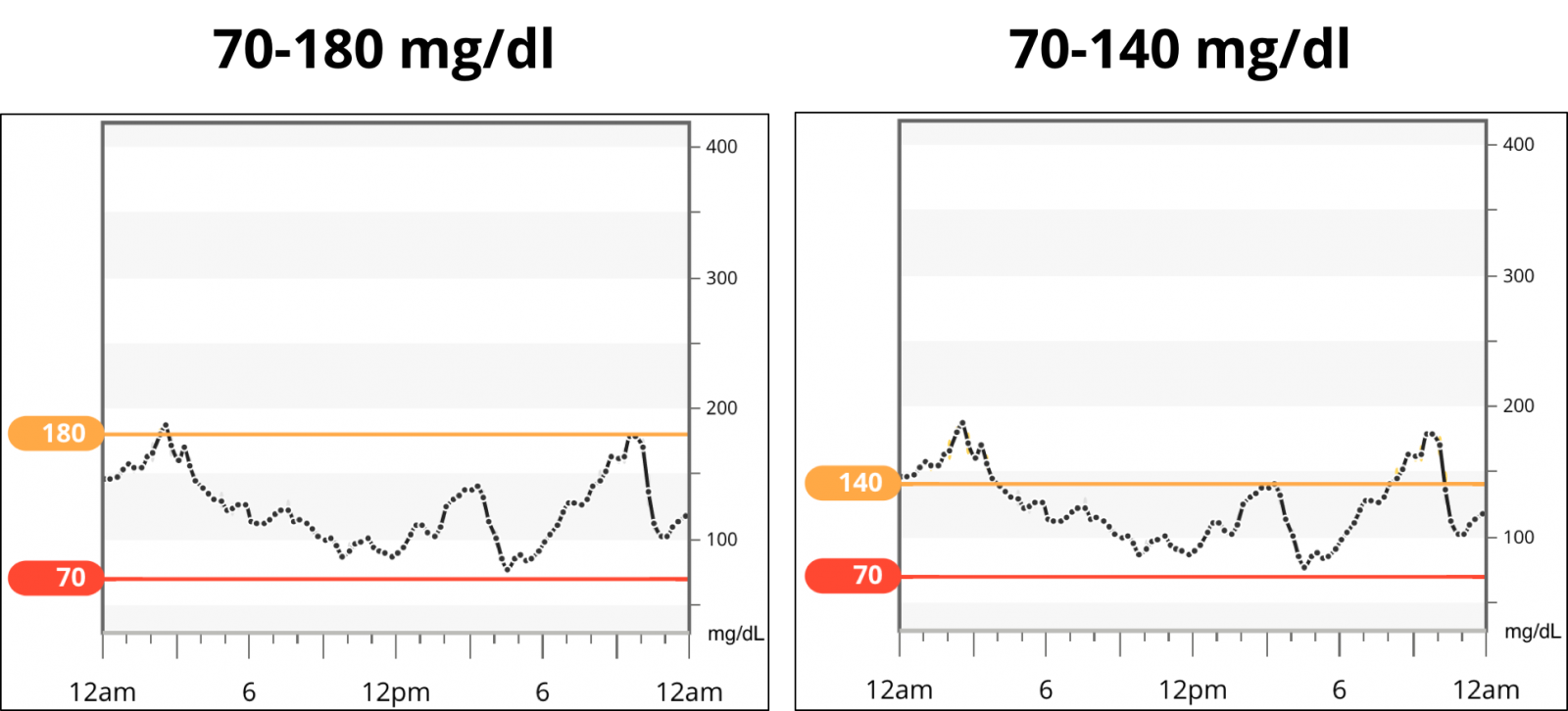
The diabetes research community has reached consensus that 70 mg/dl (low) and 180 mg/dl (high) are the lower and upper thresholds for measuring “time-in-range” when using CGM in studies – i.e., glucose readings between 70-180 mg/dl (3.9-10 mmol/l) are considered “in range,” while hypoglycemia is less than 70 mg/dl and hyperglycemia is above 180 mg/dl.
As with anything in diabetes, however, this can be individualized.
Personally, I try to aim for a tighter range of 70-140 mg/dl, in part because I have access to CGM and feel like “my best self” in this range (energy, mood, productivity, etc.). People without diabetes also typically spend most of their day in this zone, so it’s something I strive for – of course, I almost never spend 100% of any day in it.
I mention this definition upfront because the person – and the circumstances surrounding that person – defines the goal. Staying in a tighter range requires more vigilance and tools, and an achievable time-in-range for a two-year old is almost certainly different from a pregnant woman or an 86 year-old with impaired hypoglycemia awareness and no access to CGM.
How do I think about my own time-in-range? Do I have a specific goal?
In the mindset chapter of Bright Spots & Landmines, I talk about the difference between “outcome goals” and “process goals” (pages 112-115). A time-in-range “outcome” goal might be “spend X% time-in-range each day” – it is specific, and this certainly has advantages.
My approach is slightly different. I try to focus on the “process” of keeping my glucose in range each day. In other words, what key things – if I do them in the moment – will help me maximize my time-in-range? The advantage of process goals is they (i) clarify the interim steps to achieve the bigger goal; and (ii) remove many feelings of failure when unexpected things happen.
With process goals, the focus is on consistency and routine – if I get those right, the outcome often takes care of itself. Here are my big “process” goals for staying in-range:
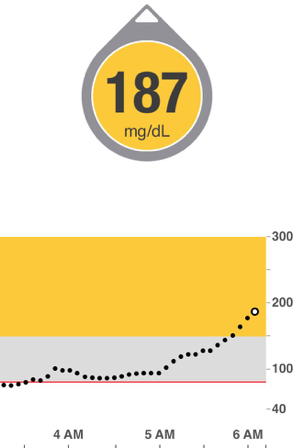 1. Get more glucose data – it’s the single most important tool for staying in range that I’ve ever discovered. As the old management adage goes, “You cannot manage what you do not measure.” For those using only fingersticks, the most important time to get glucose data (in my view) is before a meal and two hours after a meal. Another option is to wear a CGM and use the real-time trend arrows. As Dr. Steve Edelman told me, “Trend arrows are the single most important part of CGM, and they have a major influence on dosing insulin and other steps to stay in range. There is no way to stay in range without looking at the trend arrow every time you look at your CGM.”
1. Get more glucose data – it’s the single most important tool for staying in range that I’ve ever discovered. As the old management adage goes, “You cannot manage what you do not measure.” For those using only fingersticks, the most important time to get glucose data (in my view) is before a meal and two hours after a meal. Another option is to wear a CGM and use the real-time trend arrows. As Dr. Steve Edelman told me, “Trend arrows are the single most important part of CGM, and they have a major influence on dosing insulin and other steps to stay in range. There is no way to stay in range without looking at the trend arrow every time you look at your CGM.”
2. Try to minimize the biggest glucose disturbances and sources of error. For me, the most important factor has been reducing my carbohydrate intake – it dramatically improved my time-in-range (by many hours per day), subtracted most major sources of error, AND reduced my diabetes burden at the same time.
.png)
As Dr. Irl Hirsch mentioned to me via email:
“You can’t get high time-in-range when you are not careful with what you eat. Food is the key!!!”
When eating meals higher in carbs (e.g., over 30 grams), taking insulin at least 20 minutes before the first bite can really improve time in range. Carbs raise blood sugar faster than injected/pumped insulin lowers it, so the insulin head start is essential for staying in range. New faster-acting insulins, Afrezza and Fiasp, might be able to help too – ask your healthcare provider.
 3. Make “course corrections” when out-of-range blood sugars come up – e.g., taking a walk to correct a high, eating glucose tabs to recover from a low quickly. In other words, one of the best ways to maximize time-IN-range is to minimize time-OUT-of-range. Catching highs and lows quickly and addressing them helps do that.
3. Make “course corrections” when out-of-range blood sugars come up – e.g., taking a walk to correct a high, eating glucose tabs to recover from a low quickly. In other words, one of the best ways to maximize time-IN-range is to minimize time-OUT-of-range. Catching highs and lows quickly and addressing them helps do that.
4. Identify and replicate my Bright Spots – when I have a day with lots of time-in-range, what happened? How can I replicate those decisions?
5. Build routines to minimize my Landmines – when I see less time-in-range, what choices drove that? How can I avoid those decisions next time?
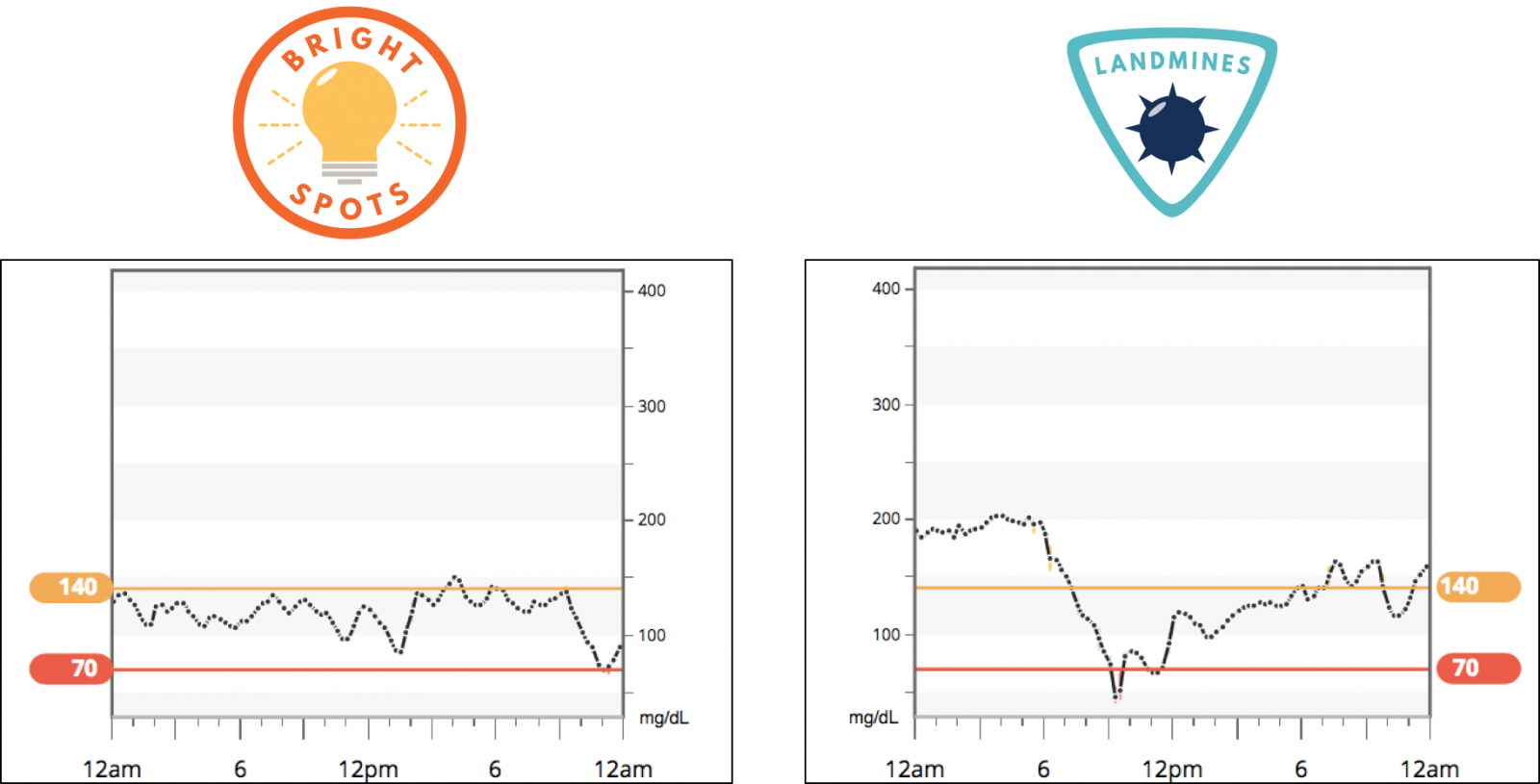
For instance, changing up my breakfast, eating an early dinner and not snacking before bed, reducing hypoglycemia binges, getting 7 hours of sleep, etc. I encourage everyone to develop their own Bright Spots & Landmines using the book’s end-of-chapter question guides.
Following these principles dramatically increases the likelihood of more time-in-range every day. Plus, it means I don’t beat myself up when I have an unexpected rollercoaster day of blood sugars.
What about specific time-in-range and time-below-range goals?
In the coming years, I hope experts debate these questions and reach a consensus on the goals for time-in-range, time-below-range, and time-above-range.
We don’t have these goals like we do for A1c, where the aim is typically less than 7% – this A1c level is based on long-term outcomes trials like DCCT/EDIC and UKPDS. Such trials are lacking for time-in-range, meaning we don’t know what the tradeoffs are – e.g., what are the relative benefits of 50% vs. 70% vs. 90% time-in-range? How do different levels of time-in-range, below-range, and above-range link to outcomes that matter?
For now, there isn’t agreement on what overall time-in-range goals should be, since everyone is so different.
.png) Dr. Roy Beck, one of the world experts on glucose data, put it well in an email to us: “Time-in-range goals depend on the individual. One should try to achieve the highest time-in-range that can be reasonably achieved, but not at the expense of an increase in hypoglycemia.”
Dr. Roy Beck, one of the world experts on glucose data, put it well in an email to us: “Time-in-range goals depend on the individual. One should try to achieve the highest time-in-range that can be reasonably achieved, but not at the expense of an increase in hypoglycemia.”
He added that good goals for hypoglycemia are “no more than 3% of the day (43 minutes) less than 70 mg/dl, and no more than 1% of the day (14 minutes) less than 54 mg/dl.” Dr. Irl Hirsch similarly recommends no more than 5% of the day less than 70 mg/dl.
Other glucose metrics can work too. Dr. Steve Edelman likes to see an average glucose of 150 mg/dl or lower, with a standard deviation (a way to measure variance from the average) of 50 mg/dl or lower. In other words, the standard deviation should ideally be less than one-third of the average glucose, indicating a tighter spread of glucose values. An advantage of this approach is it works with glucose meters too.
There are good reasons for believing that time-in-range goals need to be individualized, depending on the person and circumstances:
-
Access to tools (e.g., new medications, CGM, pumps);
-
Risk of hypoglycemia;
-
Willingness to spend time on diabetes;
-
Personal abilities (e.g., age).
For instance, as a teenager, I …
1. Took 3-4 fingersticks per day, meaning I had little data to learn and could not do “course corrections."
2. Ate a higher-carb diet that drove big spikes in blood glucose and required large insulin doses, with lots of resulting glucose disturbances and mistakes.
3. Didn’t put a lot of effort into managing my diabetes, in part because no one told me that keeping my blood sugar in range benefitted me TODAY.
I didn’t wear CGM at that time (it wasn’t available), but if I had to guess, I spent roughly 50% of the day in the range of 70-180 mg/dl. Achieving significantly higher time-in-range as a teenager would have been hard without getting more glucose data (#1) and changing my eating (#2). In other words, a single “goal” might have helped me, but my choices to achieve it are really what mattered.
What do I see in my own diabetes?
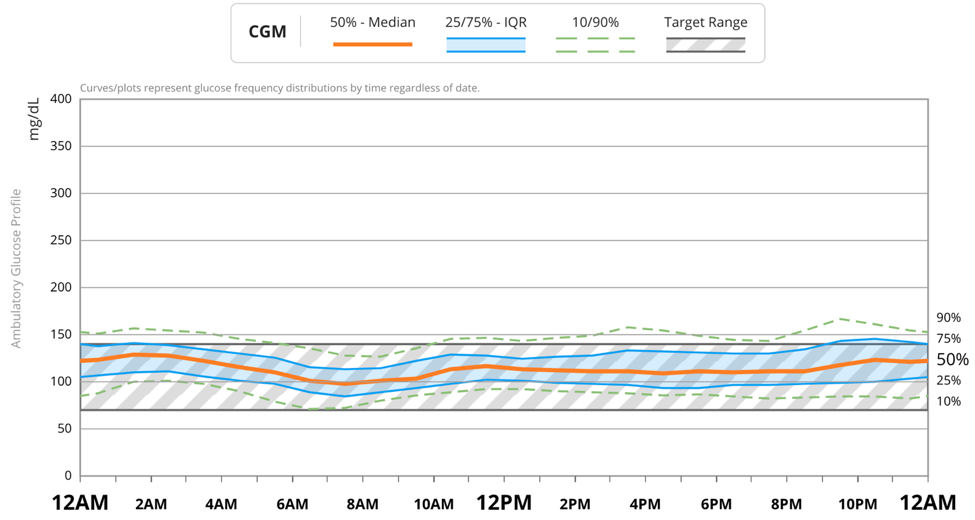
Following the principles I wrote down in Bright Spots & Landmines, I generally see approximately 70% or more of my day in the range of 70-140 mg/dl, with less than 3% time-below-range. Since experimenting with a do-it-yourself (DIY) automated insulin delivery system called Loop, I often spend around 80% time in 70-140 mg/dl, with less than 2% time-below-range. This improvement comes mostly from the overnight period, where the system is making course corrections while I’m asleep. My average glucose is typically around 120 mg/dl, with a standard deviation of around 30 mg/dl. The five tips above are the biggest time-in-range enablers, by far! Here’s my “AGP” report from the last 30 days – this “standardized” one-page CGM analysis report is now in both Abbott and Dexcom CGM:

As I noted above, I don’t set specific “goals” for myself each day, and Dr. Irl Hirsch pointed out that doing so is not always beneficial. For instance, it’s easy to become obsessive about trying to get to a specific time-in-range target, which can add diabetes burden and stress. Dr. Howard Wolpert agreed: “I always worry that focusing too much on idealized goals can set up many people with diabetes to become needlessly frustrated. When goals come up, I often qualify my suggestions: ‘When your glucoses are in range, take credit…when your glucoses are out of range, blame the diabetes and vow to make better decisions tomorrow.’”
What do recent studies show about time-in-range?
In the Medtronic MiniMed 670G pivotal study, time-in-range (71-180 mg/dl) was 72% on hybrid closed loop compared to 67% during open loop. These participants had a starting A1c of 7.4%, which improved to 6.9% on the 670G.
In the Dexcom DiaMonD study of injection users, time-in-range (70-180 mg/dl) was 51% with Dexcom CGM vs. 45% with fingersticks. These participants had a higher starting A1c of roughly 8.6%, which then improved to 7.7% with CGM.
In the Abbott IMPACT study, time-in-range (70-180 mg/dl) was 66% with FreeStyle Libre vs. 61% with only fingersticks. This was a mix of people on injections and pumps, and importantly, they had a very low starting A1c of 6.8%. However, they were spending more than three hours per day in hypoglycemia when the study began! That’s a good example of where an A1c around 7% was not of great “quality” – there was too much hypoglycemia.
In Tidepool’s Big Data Donation project, time-in-range (70-180 mg/dl) averaged 68% in the entire 354-person group, with the highest rate in 65-85-year-olds (83%) and the lowest rate in 1-5-year-olds (57%).
I find this recap fascinating, since it illustrates a few key points:
-
Access to more continuous glucose data improves time-in-range relative to fingersticks.
-
Ability to make course corrections further improves time-in-range – CGM trend arrows or use of an automated system (e.g., 670G) can help proactively avoid/limit time spent out-of-range.
-
The population of people really matters – it’s typically harder to keep time-in-range in young children vs. adults.
Questions for You
-
Do you have a time-in-range goal?
-
Have you discussed time-in-range with your healthcare provider?
-
Have you found a link between time-in-range and your mood, energy levels, productivity, etc.?
-
Have you discussed time-in-range with your loved ones, especially as it relates to your mood?
-
When you have a day with high time-in-range, what is driving that? How you can replicate those Bright Spot days?
Please share your comments here (email) or on twitter: #BeyondA1c, @asbrown1, @diaTribenews
A tremendous thanks to Kelly Close, Jim Hirsch, Dr. Irl Hirsch, Dr. Steve Edelman, Dr. Roy Beck, Dr. Robert Vigersky, Dr. Satish Garg, Dr. Tim Bailey, Davida Kruger, and Dr. Howard Wolpert for providing amazing feedback on this piece.
---
“ACTIONABLE...there are specific things you can do outlined in this book that will immediately make your blood sugars better.” – Alexis, living with diabetes and 5-star Amazon review of Bright Spots & Landmines. If you don’t have a copy yet, get it here for free or name your own price. You can also purchase it in paperback ($6), or on Kindle ($1.99). All proceeds benefit The diaTribe Foundation, a 501(c)(3) non-profit.







