What is the Gut Microbiome and How Does it Relate to Diabetes?
By Matthew Garza
 The microbiome is an exciting area of research for diabetes management. What do we know and what questions do we still have about the microbiome?
The microbiome is an exciting area of research for diabetes management. What do we know and what questions do we still have about the microbiome?
Interest in the microbiome, and how much it may affect our bodies, has been on the rise. People often talk about the microbiome as it relates to the immune system, the digestive system, chronic diseases, and more. But what exactly is the microbiome and how does it relate to diabetes?
What is the microbiome?
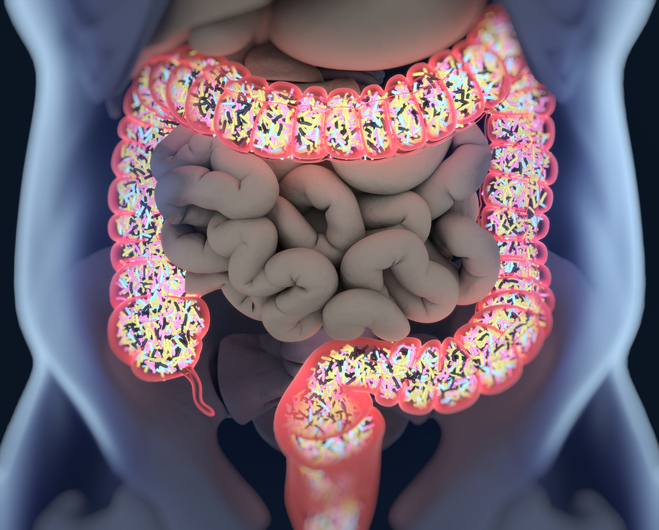
The human body is made up of tiny cells. However, we also have trillions of microorganisms (called microbiota or microbes) that are found in and on our bodies. These microorganisms include bacteria, fungi, parasites, and viruses.
While “microbiome” is defined as all the genes and DNA that these microorganisms contain, people often use the word to describe the entire population of microorganisms themselves. Even more specifically, the most common use of the word microbiome is to refer to the population of microbes that live in your gut (including your stomach and digestive tract) where the largest concentration of these microbiota can be found. While most of the microbes in the body are symbiotic (which means that both the human and the microbes benefit from the relationship), some are pathogenic, meaning that they promote diseases. In healthy individuals there is a balance between the microbes and the human host cells. If there is a major disturbance – for example, an infectious disease, the introduction of a bacteria-destroying medicine like antibiotics, or even a new diet – it can lead to the system becoming unbalanced.
Your microbiome is entirely unique to you and is determined by a number of factors including:
-
Your DNA
-
Your diet
-
Your level of activity (exercise)
-
Environmental factors – a person’s microbiome can change based on exposure (for example, to new foods or medications).
How do the microbes that make up the microbiome affect the body?
The human body needs a healthy and diverse microbiome to properly function. Our microbiomes are essential for human development, work closely with the immune system, are vital for nutrition, and even regulate how sensitive we are to insulin.
The microbiome interacts with the immune system frequently. The immune system includes all of the cells and processes in our body that fight and protect us from harmful bacteria, viruses, and disease. When germs enter the body through food or drinks, the gut microbiome plays a role in making sure we do not get sick. The microbiome also helps make vitamins and molecules that our body needs, such as B vitamins including thiamine and riboflavin, and vitamin K, among others. Microbes help break down harmful food molecules and complex carbohydrates so that the body can use the products for nutrition, muscle function, and the prevention of certain chronic diseases.
Humans share about 99.9% of their DNA (genetic material) with other humans. However, most human microbiomes are 80-90% different from person-to-person. This means that differences within the microbiome may be used for personal medicine. People respond to treatments differently for a variety of reasons, and personal medicine is a new concept for treating diabetes. If doctors know more information about the genetic makeup, or in this case the unique microbiome, of a person with diabetes, they may be able to use specific strategies for preventing, detecting, treating, or monitoring that individual’s diabetes.
How does the microbiome relate to diabetes?
Knowledge of the microbiome is limited given its relatively recent discovery. We are learning new things about the microbiome and how it relates to specific diseases, such as diabetes, every day. However, here are some of the discoveries and hypotheses being made related to the microbiome and diabetes.
For type 1 diabetes (T1D), the relationship between diabetes diagnosis and changes in the microbiome is not yet fully understood. Two studies (found here and here) highlight some of the key findings in this research:
-
People with T1D have less variety in the types of microorganisms in their microbiome.
-
Certain types of bacteria are more prevalent in people with T1D than those without – usually this means there is a smaller population of beneficial microorganisms.
-
Drastic changes in the gut microbiome could lead to a greater chance of inflammation in people with T1D. T1D is partially caused by inflammation of the cells in the pancreas where insulin is produced. Inflammation occurs when something damages your body’s cells and the immune system releases chemicals that increase blood flow and support to that area.
Similar to T1D, for type 2 diabetes (T2D) there is a lot of new research in the field, but much is still unknown. This paper summarizes many major findings:
-
Certain species of gut bacteria such as A. muciniphila can affect gut permeability, and increased gut permeability is often observed in people with T2D. Some bacteria could help decrease leaks in the gut by creating more tight junctions in our cells or by stopping the destruction of the mucin layer, a thin layer which lies on top of the inner lining of the gut. Tight junctions are small proteins between cells in the gut which prevent particles from leaking in or out.
-
Some microbes can influence blood glucose levels and control the digestion of sugars, e.g. bacteria which produce butyrate from the digestion of dietary fiber. Butyrate is a fatty acid that plays a role in homeostasis and metabolism.
-
Some microbes may affect the production and release of gut hormones, which is also highly influenced by butyrate. It has been shown that insulin sensitivity may be influenced by particular microbes.
What can you do to support the health of your microbiome?
There are a number of things you can do which have been shown to support the health of the microbiome. Here are some proactive steps you can take:
-
eating fiber (digestible and nondigestible carbs, like asparagus, onions, garlic, and chicory)
-
reducing the amount of sugars and artificial sweeteners you eat
-
avoiding taking antibiotics when not medically necessary, since this can damage your gut bacteria
-
eating plenty of fruits and vegetables
Other strategies for staying healthy also strengthen the microbiome and the immune system. These include:
-
reducing stress
-
exercising
-
getting good, quality sleep
-
not smoking at all
There are countless groups doing valuable research on the microbiome and its relationship to diabetes; however, so much is still unknown. We look forward to learning more about how to strengthen our microbiomes to keep them healthy and properly functioning.








