Sleep Apnea and Diabetes
By John Carr
 Sleep apnea can make managing diabetes more difficult. It's treated with CPAP therapy, which has also been shown to improve blood glucose control and insulin sensitivity.
Sleep apnea can make managing diabetes more difficult. It's treated with CPAP therapy, which has also been shown to improve blood glucose control and insulin sensitivity.
Sleep apnea is a common and serious medical problem that you are probably not paying enough attention to.
Sleep apnea refers to a problem during sleep where a person's airway becomes blocked. Normal breathing stops temporarily and oxygen levels fall. Since all this occurs during sleep it may go completely unnoticed.
Sleep apnea has a significant effect on health and usually gets worse if not treated. It also makes all the conditions that are important to people with diabetes – like blood pressure, glucose control, and weight – much more difficult to manage.
How could your airway become blocked during sleep?
There are three different types of sleep apnea. The most common is called obstructive sleep apnea (OSA), which occurs when the tissues that surround a person’s airway collapse and restrict airflow into the lungs.
Central and mixed sleep apnea are two other much less common types that usually occur in the setting of other serious medical problems, like stroke or heart failure.
Breathing obstruction usually occurs during a critical phase of sleep called REM (random eye movement), the period of restorative sleep when your body enters its most relaxed state. Repeated episodes of obstructed or restricted breathing that lasts for 10 seconds or more may disturb REM sleep, potentially compromising the function of the heart, lungs, and other systems in the body.
While an individual’s anatomy is an important factor in developing OSA, in persons who have excess weight or obesity, increased stores of fatty tissue surrounding the airway are important risk factors.
How does sleep apnea impact health?
The reduction in airflow in OSA causes a measurable drop in blood oxygen levels. Normally, oxygen levels during sleep remain upwards of 95%. However, in people suffering from OSA, episodes of obstruction and apnea can see this level drop below 80% for extended periods.
When a person with OSA begins to enter REM sleep and airway obstruction causes their oxygen level to fall below 90%, the body undergoes a stress response. This stress response arouses and prevents the person from entering a full REM state to help overcome the blocked airway. Untreated, this cycle repeats without ever achieving the benefits of REM sleep.
This abnormal overnight stress response from OSA disrupts normal function in multiple organ systems including the heart, circulation, lungs, eyes, and kidneys. Recent studies have demonstrated that the amount of time a person spends in this low oxygen state is directly related to the severity of associated consequences like cardiovascular disease and stroke.
In people with diabetes, this means an additional risk for complications like vision problems, peripheral neuropathy, difficulty controlling blood pressure, reduced kidney function, and decreased insulin sensitivity.
Are you at risk for sleep apnea?
The significant problem that OSA poses to people with diabetes cannot be overstated. Estimates reveal that about 18% of all people with type 2 diabetes have OSA. As people grow older or gain weight, the likelihood of OSA greatly increases.
Research shows that there also appears to be a two-way relationship between diabetes and sleep apnea; people with diabetes are more likely to get OSA, and OSA is a contributing factor in developing diabetes.
Other risk factors for OSA include:
-
Smoking
-
Alcohol or sedative use
-
Obesity
-
Aging
-
Narrow airway
-
Nasal congestion
Signs and symptoms of sleep apnea
The most common symptoms of sleep apnea are excessive fatigue and daytime sleepiness. If you have a history of falling asleep on the job, during conversations, or when driving it’s a strong indication further evaluation is needed.
A person suffering from obstructive sleep apnea will often be witnessed by a partner or family member snoring heavily or gasping for air when sleeping.
Is there a test for sleep apnea?
The test to evaluate for OSA is a sleep study that determines the frequency and severity of apnea episodes.
This test can either be done at a sleep facility or home. Measurements may include an ECG, oxygen levels, muscle movements, airflow, and other parameters during sleep that assist in detecting and counting apnea events.
Here’s how OSA is graded (meaning the number of events per hour):
-
Normal: Less than five per hour
-
Mild: Between 5-15 per hour
-
Moderate: Between 15-30 per hour
-
Severe: Greater than 30 per hour
With the introduction and rapid improvement of wearable technology, several new products in development may offer easier, cheaper, and more accurate assessments.
One example is from Sunrise, a company that develops sleep monitoring technologies. The Sunrise technology is a small device that can be used at home to detect muscle contractions in the jaw during sleep, a marker of OSA.
“There is a real push in this space to be able to accurately determine who has treatable disease,” said Chandler Miller, a bioengineer who works with Sunrise. “Some of these new technologies will be able to better quantify the burden, or to better track changes over time.”
Miller added that such tech opens up all types of potential to improve CPAP fitting and optimization, plus a more nuanced understanding of the effects and benefits.
How is sleep apnea treated?
Sleep apnea treatment involves a specialized breathing machine called continuous positive airway pressure (CPAP). CPAP devices keep your airway open during sleep and are the most effective treatment and thus are first-line therapy for OSA.
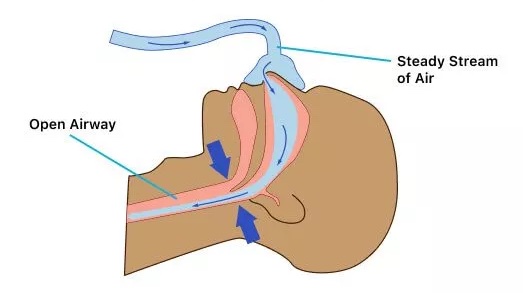 A useful way to understand how CPAP works is to imagine yourself in a moving car with your head held outside the window; the wind pushing its way into your lungs is CPAP. Treatment with CPAP requires a small bedside medical device and a sealed mask worn over the nose or mouth while sleeping. This setup delivers air at a set pressure and monitors breathing through plastic tubes.
A useful way to understand how CPAP works is to imagine yourself in a moving car with your head held outside the window; the wind pushing its way into your lungs is CPAP. Treatment with CPAP requires a small bedside medical device and a sealed mask worn over the nose or mouth while sleeping. This setup delivers air at a set pressure and monitors breathing through plastic tubes.
Airway collapse occurs at the end of an exhale (out breath) and the beginning of inspiration (in breath) when lung and airway volumes are at their lowest point. However, the collapse is prevented by the continuous gentle airflow, sometimes with well-timed “puffs” of air, during that vulnerable period.
In rare circumstances, surgical procedures may assist with the management of severe OSA. For the vast majority, lifestyle modifications (like exercise and weight loss) and CPAP machines are the most effective for treating sleep apnea.
How effective is treatment?
CPAP is very effective to treat sleep apnea, said Dr. Douglas Beach, a critical care and pulmonology specialist at Beth Israel Deaconess Medical Center and instructor of medicine at Harvard Medical School who specializes in treating sleep disorders.
However, he said, about 50% of people have difficulty accepting the treatment and then only about 40% continue treatment past three weeks as CPAPs can be cumbersome and uncomfortable.
“If a person is able to use the CPAP device, they can have a dramatic improvement in symptoms of fatigue and sleepiness, as well as improvements in blood pressure, reductions in heart disease, and improvement in kidney function,” Beach said.
“There are a number of ongoing trials that will help us understand how good this therapy is, but the sticking point continues to be compliance. Recent advances in masks and the PAP devices have helped make this therapy more comfortable, but it takes getting used to,” he said.
Especially important to those with diabetes, CPAP therapy can improve insulin sensitivity and blood glucose control, an effect observed in people with diabetes, prediabetes, and individuals without diabetes.
For those unable to tolerate CPAP, the Inspire implant may be an option. It delivers gentle pulses to airway muscles to keep the breathing passage open so the person with OSA can breathe regularly and sleep soundly.
What can I do to avoid developing sleep apnea?
Lifestyle changes are an important component of diabetes care and this is no different with OSA. Actions you can take to avoid or at least delay the development of obstructive sleep apnea are lifestyle modifications including weight reduction, improved glucose control, eating a healthy diet, and stopping tobacco and alcohol use.
The bottom line
Getting a good night's sleep is essential for everyone. Sleep apnea can significantly impact various aspects of your health, including blood pressure, glucose levels, and weight management, making it particularly challenging for individuals with diabetes.
Early detection and appropriate treatment of sleep apnea, primarily through therapies like CPAP, are crucial in mitigating these risks and improving overall health outcomes. By addressing sleep apnea alongside diabetes management, people with diabetes can ensure better health.








